Dementia: The Right Prescription
Published on behalf of Katie Clark, Dementia and Elderly Care Project Manager.
The Dementia Action Alliance (which includes organisations such as Alzheimer’s Society, Age UK and Bupa) has launched a call to action on the use of antipsychotic drugs for people with dementia.
The prescription of anti-psychotic medication to people living with dementia has long been debated. Often these drugs are seen as a solution to behavioural and psychological symptoms of dementia like distress or agitation, but can end up causing more damage, creating ‘mobility problems, sedation and sometimes death, particularly when used for longer than 12 weeks’. The Alliance is careful to point out that,
‘In some cases the use of antipsychotic drugs is the right treatment option, but it is estimated that around two thirds of the use of antipsychotics in people with dementia is inappropriate.’
In light of this, they are calling for a review of all prescriptions for antipsychotics by the end of March 2012. To put that in context, around 180,000 people with dementia are thought to be prescribed antipsychotic drugs in the UK, so that is a big job, but if the figures are correct, it also means that up to 120,000 people are being prescribed the drugs who shouldn’t be, so drastic action is needed.
Jeremy Hughes, Chief Executive of the Alzheimer's Society, said
"It's not just about reducing antipsychotics but also about improving quality care. This means developing alternative treatments and finding better ways to manage pain and other medical conditions."
The Reader Organisation has been delivering reading groups in care homes and working with people living with dementia, staff and family carers since 2006. Our work links directly to the National Dementia Strategy’s objective to improve the quality of care by providing meaningful engagement. In a recent evaluation we found that during groups :
- 86% of members are less agitated
- 86% have improved mood
- 87% have improved concentration
- 73% have better social interaction.
We also found that some of these outcomes continue long after the group is over, such as less agitation and improved mood.
We are currently halfway through a pilot project with Bupa Care Homes delivering GIR groups with residents and training staff members up to use shared reading with those they work with. In a group last week a very distressed and agitated lady wandered in towards the end of the session. (I will call her M.) I had seen her before and noticed that she was often alone, and never seemed to settle in one place, but moved around constantly, walking up to people, shouting at them and pointing, and then walking away again. Her language is very confused and it is difficult to understand what she says, and other residents seem unsure of her and keep their distance. When she first came into the group, she banged her fist on the table and shouted something very loudly, then she grabbed one of the poems from the top of the pile and looked at it very closely. I took this opportunity and quickly handed round copies of that poem to the rest of the group.
We then read it aloud together. M found an empty seat around the table and sat down, still looking at the poem. She didn’t say anything and didn’t read aloud, but her eyes were scanning across the lines as if she was reading it in her head. She sat for 10 minutes until the end of the session, and at the end, got up and waved and smiled to the other group members.
This week when I returned, M was ready. She came straight into the group and sat in the same seat. She eagerly took the poems and when we read one about evacuation, clearly said ‘I was’. She stayed for over an hour, reading and listening to the poems, watching and listening to other group members talking about them and their own experiences and even joining in herself with the discussion. She was calm, peaceful and smiled a lot during the session. I think M’s experience demonstrates the way in which the power of language and the rhythms of poetry can soothe and calm, and also remove barriers in bringing people together. It was wonderful to see M enjoying herself and to see other residents listening to her and encouraging her.
Watching this video on the BBC’s news website has strengthened my resolve to spread the use of GIR in care homes and hospitals and I hope that this review will not only reduce the incorrect use of anti-psychotic drugs, but will result in improved quality of care going forward. 120,000 is a very large number of reviews, but hearing Michael’s story here brings home the fact that each one of those could have a huge impact on the life of the person with dementia and all those that love and care for them.
Share
Related Articles

The Reader’s gardening group calls for more volunteers
The Reader would like to thank the incredible hard work, dedication and energy of its volunteer gardening group for transforming…
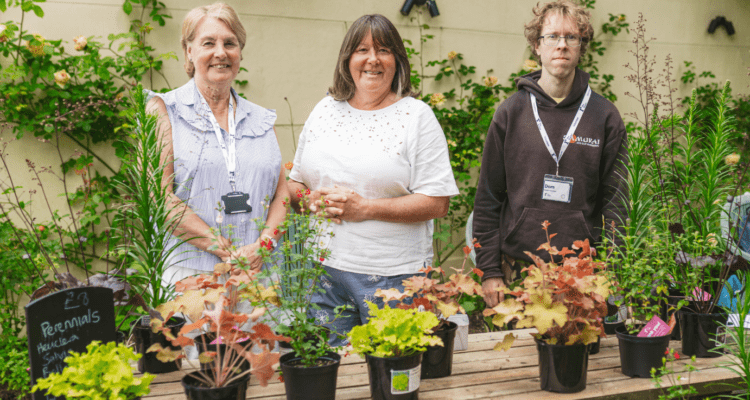
Meet The Reader’s volunteer gardeners
Three of our amazing volunteers reveal why they joined and what they enjoy about the group, including Paula Ross who…

“I am always surprised how much better I feel” Elaine’s Volunteering Story
When Elaine retired from her busy job in the NHS she looked for opportunities to spend more time outdoors. Following…


1 thoughts on “Dementia: The Right Prescription”
[…] settings should be considered ‘integral’ rather than ‘additional’. In her recent article, Katie Clark spoke of the positive impact Get Into Reading has had on people suffering from […]